The ability to rapidly and accurately assess the neurological status of a patient in critical care environments is critical. Effective assessment tools are important because studies show that timely detection of neurological change can cut death rates by up to a third in critically ill patients. The pupillary light reflex, a straightforward but very reliable indicator, is of paramount importance in uncovering disorders of the neurological order. It is important for healthcare providers to know how the reflex works and how to measure it, using up-to-date technology of a pupillometer in the Neuro exam setting.
What Is the Pupillary Light Reflex?
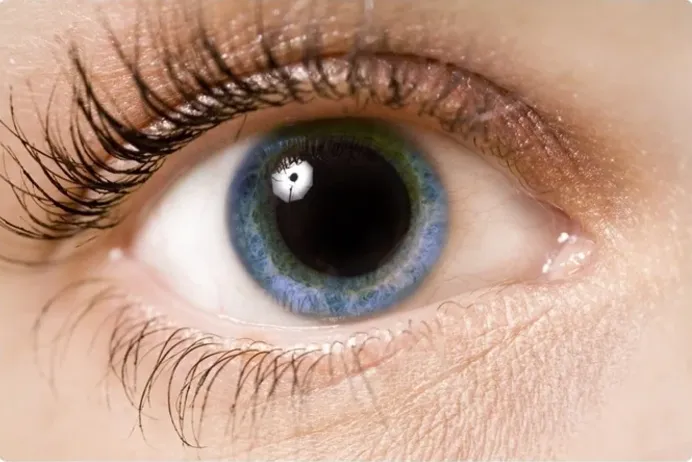
The pupillary light reflex is a fundamental physiological response to light by which the pupil constricts. This response occurs due to neural pathways that control pupil size: when light hits the retina, that causes an impulse to travel down the optic nerve to the brainstem which in turn tells the pupil to constrict. This is a reflex action and is hence entirely involuntary, what that means is that it does not involve any conscious control whatsoever, it works in a certain autonomic manner of the body.
Pupil constriction may seem simple, but it’s actually quite complicated. This reflex is an important indicator of neurological health, and abnormalities may indicate problems with brain injuries and strokes to the more hidden and subtle neurological disorders.
Why the Pupillary Light Reflex Matters in Critical Care Nursing?
For a critical care nurse, the pupillary light reflex is far more than a routine observation—it is a vital insight into the brainstem, the controller of essential life-sustaining functions like breathing and heart rate. This reflex plays a crucial role in diagnosing brain dysfunctions, such as increased intracranial pressure, which may signal serious conditions like brain hemorrhages or traumatic brain injuries.
In the high-stakes environment of critical care, every second matters. A neuro exam that includes assessing the pupillary light reflex can provide early, potentially life-saving indications of neurological decline, paving the way for timely intervention and treatment. A sluggish or absent pupil reaction isn’t just a minor detail—it’s often the first red flag of a more serious underlying issue within the brain, highlighting the critical importance of this assessment in patient care.
The Pupillometer
Traditionally, the pupillary light reflex is observed manually using a flashlight. Today, however, advancements in technology have equipped healthcare providers with neurological tools like the pupillometer, allowing for far more precise measurements of pupil size and reaction speed than the human eye can achieve.
The pupillometer not only enhances accuracy but also eliminates variations that can occur with subjective human observation. This device provides quantitative, objective data, enabling healthcare professionals to monitor subtle changes in a patient’s neurological status over time. With the pupillometer, critical care nurses can track the condition of post-operative brain surgery patients or individuals recovering from traumatic injuries with a level of precision and consistency that manual observation simply cannot match. This objective insight aids in identifying early signs of complications, supporting timely intervention when it matters most.
How Abnormal Pupillary Responses Indicate Neurological Disorders
An abnormal pupillary light reflex can signal a range of neurological disorders. For instance, a sluggish or absent pupil constriction in response to light might indicate damage to the optic nerve or brainstem. Conditions like brainstem injuries can disrupt the neural pathways necessary for a proper pupillary response, leaving behind a critical clue visible in the eyes.
Additionally, asymmetry between pupils—known as anisocoria, where one pupil is larger than the other—may point to serious conditions such as a stroke or brain hemorrhage. These conditions can create pressure on the brainstem, altering the way each pupil responds to light. This subtle difference, often detectable only through careful assessment, serves as an important diagnostic marker for healthcare providers monitoring neurological health.
Conclusion
The NPI pupillometer serves as a gateway to understanding a patient’s neurological health. Detecting subtle changes in the pupillary light reflex enables the early identification of critical conditions such as brain injuries and strokes. Timely recognition of these issues can lead to faster interventions, potentially saving lives. This underscores the profound value of seemingly small physiological signs like the pupillary response, which can offer crucial insights that guide life-saving decisions in clinical practice.